Health & Society
Scientologists Lead Human Rights Advocacy in Mental Health Through CCHR Exhibition in the Netherlands

Netherlands – February 18, 2025 – The Netherlands Committee for Human Rights Foundation (NCRM), in collaboration with the Citizens Commission on Human Rights (CCHR), successfully hosted the traveling exhibition “Psychiatry: An Industry of Death” at the Zuiderkerk in Amsterdam. This powerful event, held from February 15 to 17, shed light on historical and contemporary human rights violations within psychiatry. The exhibition, driven by the dedicated efforts of Scientologists and human rights activists, provided an eye-opening experience to hundreds of visitors.
The three-day exhibition took place in the heart of Amsterdam, a striking contrast to a concurrent European Congress of Neurology and Neuropsychiatry, which was held in a secluded industrial area outside the city. This strategic placement of the exhibit ensured maximum public visibility and accessibility, reflecting the transparency and public engagement that CCHR stands for.

An Eye-Opening Journey Through Psychiatry’s History
Visitors to the exhibit were guided through interactive displays, multimedia presentations, and historical accounts that detailed psychiatry’s troubled past, from early psychiatric institutions and eugenics programs to modern-day concerns like over-medication and involuntary commitment. The powerful visuals and testimonies resonated with the hundreds of visitors who attended, ensuring that critical discussions on psychiatric practices remained in the public domain.
The Zuiderkerk, a historic site that once served as a cemetery, added a symbolic weight to the event. The entrance porch, marked by a skull and crossbones, served as a stark reminder of the suffering endured by victims of psychiatric abuse. Volunteers ensured that CCHR’s message was visible throughout—from a balloon arch in CCHR colors to informational boards and flyers distributed on-site.
Exposing Psychiatric Practices and Their Consequences
The exhibition coincided with the psychiatric congress, whose program included sessions on brain stimulation techniques, including electroshock, electromagnetic induction, and deep brain stimulation via implanted electrodes. NCRM volunteers emphasized that while some neurotechnological treatments may help patients with nerve damage, psychiatry’s historical focus on biochemical imbalances and brain interventions has led to an alarming rise in psychiatric drug prescriptions, now affecting nearly 3 million people in the Netherlands.

A key issue highlighted was the sharp increase in ADHD diagnoses and the use of Ritalin, which quadrupled after a 2005 treatment guideline heavily influenced by psychiatrists with pharmaceutical industry ties. Today, nearly 4% of Dutch youth are medicated for ADHD, despite experts pointing to social and environmental factors—such as school pressure, poverty, and screen exposure—as major contributors to behavioral difficulties.
Stories of Strength and Survival
A particularly moving moment came when a survivor of psychiatric institutionalization, bravely shared her experience. She recounted how she was forcibly taken from her home, denied access to her children, and placed under psychiatric incarceration, where every attempt to assert her rights was met with further drugging and control. She revealed that the only way to escape was to pretend to comply—a sentiment echoed by another visitor who had faced similar struggles.
The official opening of the exhibition featured another powerful testimony from an expert by experience, who described her forced admission and the emotional toll it took on her. Her account deeply moved the audience, many of whom admitted they were previously unaware of the extent of such abuses in psychiatry.
Electroshock Therapy and the Call for Reform
A crucial topic in the exhibition was electroshock therapy (ECT), which is still performed on 1,000 patients annually in the Netherlands. Despite mounting evidence of its permanent memory loss risks and lack of proven efficacy, psychiatric institutions continue its use. A controversial study on ECT in 2020 led to the following conclusion: “Given the high risk of permanent memory loss and the small mortality risk, this longstanding failure to determine whether or not ECT works means that its use should be immediately suspended until a series of well-designed, randomized, placebo-controlled studies have investigated whether there really are any significant benefits against which the proven significant risks can be weighed“. Apparently, “criticism is not or hardly getting through to the psychiatric caste” says Ivan Arjona from Scientology Europe, who has been involved since years at the UN denouncing the heavy violations of human rights. The UN Special Rapporteur on Torture even stated that forced psychiatric interventions could amount to torture when imposed without true informed consent.
NCRM volunteers pressed the Dutch Association for Psychiatry for a response, but the association defended its adherence to existing laws and regulations rather than reconsidering its stance. This highlights the persistent institutional resistance to reform, despite growing global advocacy from the WHO and UN for a shift away from the biomedical model of mental health.
The Role of Media in Amplifying the Message
The exhibition’s impact was further strengthened by media coverage, which played a key role in bringing awareness to the broader public. Reports appeared in “De Andere Krant”, an alternative Dutch newspaper with 12,000 prints, as well as in Amsterdam Daily, ensuring that the issues raised reached a wider audience. Additionally, the open letter addressed to the psychiatry congress organizers had tangible effects. In response to CCHR’s advocacy, the congress removed two key sessions on brain stimulation techniques and pharmacological treatments—a significant victory in the fight against coercive psychiatric interventions.
CCHR volunteer Ogé further emphasized the importance of implementing WHO and UN guidelines that promote ethical mental health practices, highlighting CCHR’s ongoing role in shaping policies that safeguard human rights.
A Continuing Fight for Mental Health Rights
Since its founding in 1969 by members of the Church of Scientology, inspired by the work of L. Ron Hubbard, and psychiatrist Dr. Thomas Szasz, CCHR has remained a leading voice in exposing psychiatric abuses and advocating for reforms. Through public exhibitions, legal actions, and lobbying efforts, CCHR continues to challenge the pharmaceutical industry’s influence, prevent coercive treatments, and defend the rights of individuals affected by psychiatry.
The success of the Amsterdam exhibit is a testament to the unwavering dedication of Scientologists and CCHR activists in bringing truth and accountability to the field of mental health. As the battle for human rights in psychiatry continues, CCHR’s work stands as a beacon of hope and justice for individuals and families affected by psychiatric abuses.
Health & Society
CCHR Encourages Italy to Complete Full Mental Health Reform After Court Ruling on Forced Treatment

KINGNEWSWIRE / PRESS RELEASE / ROME — In what has been widely reported as a landmark decision, Italy’s Constitutional Court struck down portions of the nation’s decades-old psychiatric treatment laws in May 2025, declaring unconstitutional Article 35 of Law 833/1978. The ruling affects procedures for Trattamento Sanitario Obbligatorio (TSO), the legal framework governing compulsory psychiatric hospitalization. While many media outlets have hailed the move as progress, critics—including prominent human rights advocates and civil society organizations—warn that the ruling fails to fully align Italy’s mental health practices with modern international human rights law.
At the heart of the decision is the acknowledgment that individuals subjected to TSO must be notified of the order, granted access to legal counsel, and given the opportunity to present their case before the Tutelary Judge prior to judicial validation. However, the Court did not abolish TSO itself, instead choosing to preserve the practice with additional procedural safeguards.
This approach has drawn sharp criticism from those who argue that forced psychiatric treatment is inherently incompatible with human dignity and the right to autonomy.
A Bit Closer but not yet in Full Compliance with International Standards
The United Nations Convention on the Rights of Persons with Disabilities (CRPD), which Italy ratified in 2009, explicitly rejects coercive interventions in mental health care. General Comment No. 1 from the CRPD Committee affirms that all persons, regardless of disability status, have the right to legal capacity and must be supported—not substituted—in making decisions about their lives and bodies.
In recent years, the Office of the UN High Commissioner for Human Rights (OHCHR) and the World Health Organization (WHO) have echoed this stance, calling for the complete abolition of forced psychiatric interventions and urging nations to adopt support-based, rights-respecting alternatives.
An April 2025 WHO report titled “Countries move away from using coercive measures in mental health care” emphasized that seclusion, restraint, and involuntary treatment are not only harmful but also violate human rights under all international instruments, including the CRPD. The report concluded:
“Forcibly restraining or secluding someone who is experiencing a mental health crisis can lead to severe physical injury and even death. People who have experienced these coercive measures say that they are traumatic, detrimental to recovery and engender mistrust in mental health services. They are systemic failures of care.”
Despite these global developments, the Italian Constitutional Court’s ruling stops short of eliminating TSO. Instead, it upholds the legality of involuntary psychiatric treatment while introducing modest reforms to how such measures are applied.
CCDU: Longtime Advocates for Dignity and Autonomy
The Citizens Commission on Human Rights Italy (CCDU), the Italian branch of the organization founded by the Church of Scientology in 1969 and long active in exposing abuses within psychiatry, has consistently advocated for the full decriminalization of mental distress and the dismantling of institutionalized coercion in mental health care.
CCDU praised the procedural improvements mandated by the Court but warned that allowing any form of forced treatment remains a grave ethical and legal failure.
“Dignity cannot be conditional,” said a CCDU representative. “If we recognize people as equal citizens, then they must have the right to make choices—even when others disagree with them.”
Since its founding, CCHR worldwide has worked alongside survivors, whistleblowers, and international partners to document systemic abuses in psychiatric facilities and push for transparency in clinical settings.
In line with this CCDU in Italy has backed a legislative proposal introduced by the advocacy group Diritti alla Follia, which seeks to replace TSO entirely with voluntary, community-based care models grounded in informed consent.
This support draws directly from the principles laid out by L. Ron Hubbard, founder of the Church of Scientology. Hubbard was a fierce critic of coercive psychiatry, and his writings formed the philosophical foundation for CCHR’s global campaign to end involuntary mental health interventions.
Today, CCHR continues that legacy, working closely with international watchdogs like the European Committee for the Prevention of Torture (CPT) and the UN Special Rapporteur on Torture, the UN Office of the High Commission on Human Rights (OHCHR) and various UN Human Rights Treaty bodies.
Why TSO Remains a Violation—No Matter the Process
Human rights watchdogs, including the CPT and the OHCHR, have repeatedly condemned practices involving non-consensual psychiatric treatment. The CPT specifically have argued that even with due process, forced medication and detention violate Articles 7 and 9 of the European Convention on Human Rights. Article 7 is centered around the principle of No punishment without law while Article 9 provides a right to freedom of thought, conscience, and religion. The OHCHR and other UN Human Rights treaty bodies stress that coercion in psychiatry violations of human rights under all international instruments, including the United Nations Convention on the Rights of Persons with Disabilities.
The CPT has specifically called out Italy for its reliance on TSO and urged authorities to develop alternative models that respect personal autonomy and informed consent.
Moreover, the OHCHR and WHO all encompassing Mental Health, Human Rights and Legislation: Guidance and Practice emphasizes that countries should move away from institutionalization and coercion, and instead invest in peer support, crisis homes, and community-led services.
“The idea that someone can be forcibly hospitalized and medicated simply because they think differently is archaic,” said Ivan Arjona, Scientology’s Representative to the Europen institutions and the United Nations. “It’s a good opportunity for Italy to go all the way forward and ensure full embracement of the human rights model in Mental Health.”
What Comes Next?
With the Constitutional Court’s decision now in force, Parliament faces the task of drafting new legislation to replace the unconstitutional provisions. While some lawmakers have signaled openness to reform, others remain aligned with traditional psychiatric institutions and clinical interests.
Meanwhile, the Ministry of Health reports that over two million Italians lack access to adequate mental health care, and emergency departments have seen a surge in psychiatric crises—an alarming trend that underscores the need for systemic change.
The CCDU and allied groups warn that without a clear commitment to abolishing coercion, any new legislation will perpetuate the very violations the Court claims to address.
“We’ve seen this before,” said a spokesperson from the CCHR European office. “Governments add layers of procedure to give the illusion of protection, but the core violation—the denial of bodily integrity and freedom—remains intact.”
As Italy stands at this crossroads, the question is no longer whether the system needs to change, but whether it has the political will to break free from outdated paradigms of control and embrace a future rooted in human rights, dignity, and true healing.
References:
Constitutional Court of Italy – Decision on Article 35 of Law 833/1978 (May 2025)
United Nations Convention on the Rights of Persons with Disabilities (CRPD) UN CRPD Treaty Page
UN Committee on the Rights of Persons with Disabilities – General Comment No. 1 (2014)
- CRPD/C/GC/1 – Full Text
Office of the UN High Commissioner for Human Rights (OHCHR)
World Health Organization (WHO) – April 2025 Report: “Countries move away from using coercive measures in mental health care”
**WHO/OHCHR Publication – “Mental Health, Human Rights and Legislation: Guidance and Practice” https://www.who.int/publications/i/item/9789240080737
Health & Society
From Asylums to Psychopharmaceuticals: Italy’s Struggle for Mental Health Rights
In a society increasingly aware of mental health issues, the line between treatment and coercion remains disturbingly blurred — especially in Italy, where a decades-old reform has been both praised and criticized as outdated in the face of new challenges.
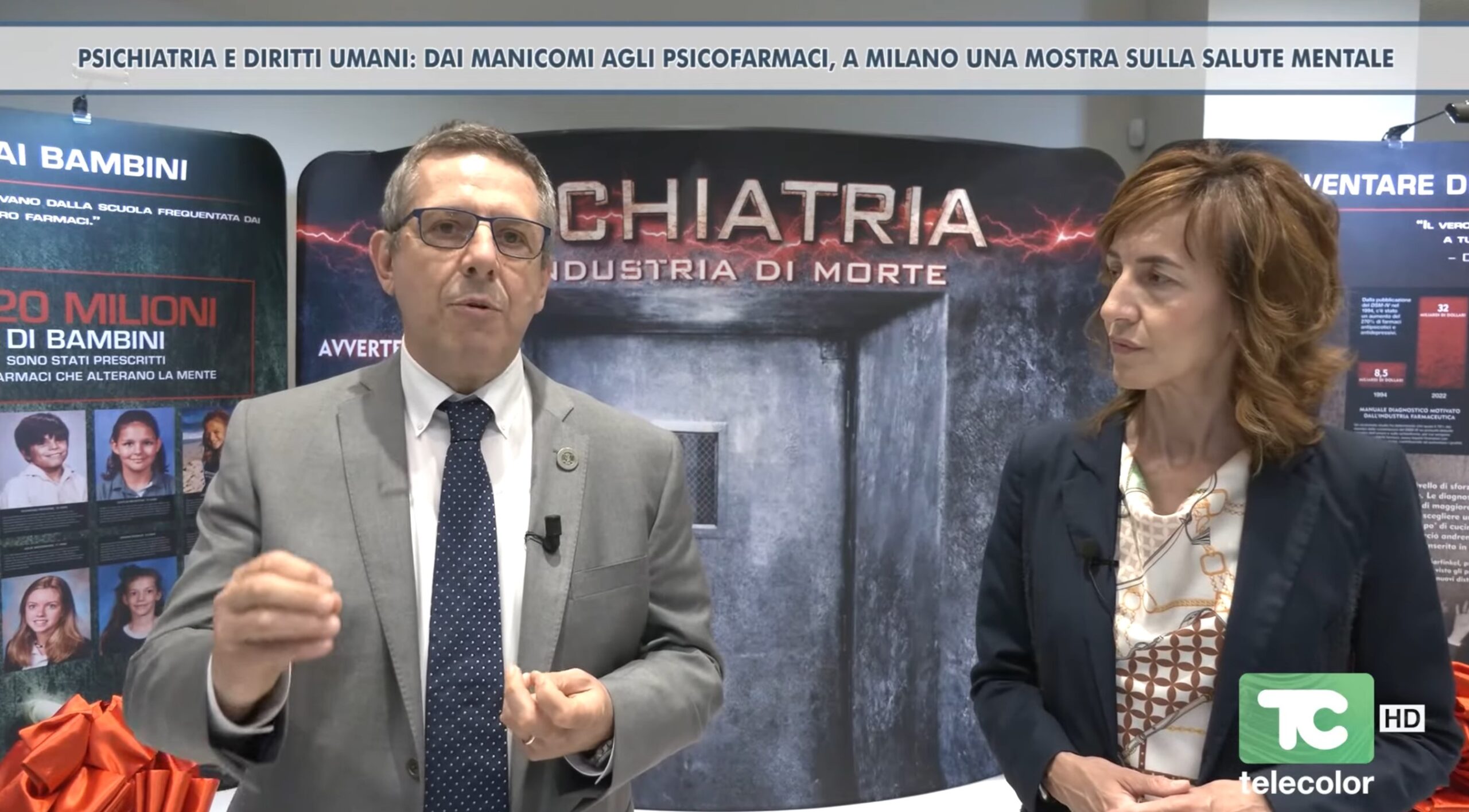
A recent exhibition in Milan, “Psychiatry and Human Rights: From Asylums to Psychopharmaceuticals,” revisits the long and often troubling history of mental health care — from the horrors of Nazi concentration camps and Soviet gulags, through the rise and fall of electroshock therapy and psychosurgery, to the landmark 1978 Basaglia Law, which closed psychiatric hospitals across the country.
The exhibit, organized by the Citizens’ Committee for Human Rights (CCHR Italy), not only documents this evolution but also raises urgent questions about contemporary practices — particularly the use of compulsory psychiatric treatment under Italy’s current legal framework.
“This exhibition aims to inform professionals — doctors, psychologists, social workers, lawyers — as well as the general public about a serious situation that exists in Italy, and indeed globally, regarding mental health,” said Alberto Brugnettini, Vice President of CCHR Italy , during an interview on TeleColor . “It’s a historical documentation of psychiatry from its origins to today, including all the mistakes of the past, up to modern times — including the so-called Basaglia Law.”
Named after psychiatrist Franco Basaglia, the law was intended to revolutionize mental health care by closing down asylums and promoting community-based treatment. But according to critics like Brugnettini, it never fully lived up to its ideals.
“In reality, the law wasn’t even written by Basaglia,” Brugnettini explained. “It was drafted by Bruno Orsini, a Christian Democrat psychiatrist and politician, and passed against Basaglia’s own objections. He opposed coercive treatments and feared that transferring authority from asylums to hospital wards would simply recreate the same oppressive logic inside new structures — a fear later confirmed by Italy’s Court of Cassation 50 years later.”
Indeed, the Italian Supreme Court recently ruled that the current system of Trattamento Sanitario Obbligatorio (TSO) — or mandatory psychiatric treatment — may violate constitutional rights. In an unprecedented move, the Court referred several articles of the law to the Constitutional Court, stating that they may be unconstitutional.
“The Constitution guarantees the right to health,” Brugnettini noted, “but the Court of Cassation has now affirmed that the right to freedom carries equal weight. It is unacceptable to deprive someone of their liberty without giving them the chance to express their reasons before a judge — perhaps with legal representation.”
International human rights bodies, including the United Nations , the World Health Organization , and the European Committee for the Prevention of Torture , have also raised concerns over Italy’s use of involuntary psychiatric interventions.
Guidelines jointly published by the UN High Commissioner for Human Rights and the WHO call for the replacement of what they describe as the “biological, mechanistic, and coercive” model of mental health care with one that is “humanistic, holistic, and respectful of human rights.”
Yet in many cases, the opposite appears to be happening.
According to Brugnettini, patients labeled as “voluntary” are sometimes coerced into signing consent forms under the threat of forced treatment — a practice the European Committee for the Prevention of Torture has condemned.
“They say, ‘Come in willingly or we’ll bring you in by force,’” he said. “So people sign, thinking they’re making a choice. But when they decide to leave, they’re restrained. That’s not voluntary. That’s coercion.”
The exhibition also highlights the continued use of controversial procedures such as electroconvulsive therapy (ECT) — commonly known as electroshock — despite growing international criticism.
“There are still four or five cities in Italy where ECT is used,” Brugnettini said. “While there is a ministerial circular — the Bindi Circular — that limits its use, we suspect that informed consent is not always truly informed. Patients may not be fully aware of the risks involved.”
He added: “Even psychiatrists struggle to explain why inducing seizures should be therapeutic. There’s no scientific consensus on how it works, yet it’s associated with memory loss, cardiovascular risks, and in some cases, even death.”
The exhibit features profiles of famous figures who suffered under psychiatric care — including Ernest Hemingway , who died by suicide after undergoing multiple electroshocks and wrote in his final letter that the treatment had “cured the illness but erased my memory,” and Marilyn Monroe , whose death was linked to barbiturate overdose.
Brugnettini argues that these stories illustrate a broader issue: the tendency to label complex human behaviors as medical disorders without biological evidence.
“In psychiatry, symptoms, signs, and diagnosis are often the same thing,” he said. “For example, if a child is diagnosed with ADHD, the symptoms are hyperactivity and inattention — and those are also the signs and the diagnosis. There’s no objective test, no blood work, no scan. These are labels applied to behavior, often based on subjective criteria.”
He pointed to the DSM-5 , the American Psychiatric Association’s diagnostic manual, which lists more than 368 mental disorders — each approved by vote rather than empirical research.
“We’re not anti-psychiatry,” Brugnettini clarified. “We’re pro-human rights. Our message is clear: reform the TSO law, restore justice, and align Italian mental health policy with international standards.”
As debates around mental health grow louder across Europe, Italy finds itself at a crossroads — caught between legacy and reform, between treatment and control.
And in that tension lies a fundamental question: When does care become coercion?
Health & Society
Proactive Steps To Ensure Health Security In European Politics

Most people underestimate the integral role health security plays in European politics. In a landscape fraught with health crises and political instability, it is imperative that you take proactive steps to enhance this security. By understanding the interconnectedness of health policies, governmental actions, and public trust, you can contribute to a more resilient future. Adopting measures such as promoting international cooperation, strengthening healthcare systems, and prioritising mental health will not only safeguard your community but also foster stability across Europe.
Understanding Health Security
Before addressing the intricacies of health security in European politics, it is crucial to grasp what health security entails. Health security primarily involves the protection of populations from health threats, including infectious diseases, environmental hazards, and bioterrorism. It not only concerns individual health but also the broader social and economic stability that can be undermined by health crises. The importance of health security becomes evident when you consider how interconnected our societies are; a health threat in one region can quickly escalate to affect others, underscoring the need for collaborative strategies to mitigate potential risks.
Definition and Importance
The term ‘health security’ signifies far more than just the absence of disease. It encompasses the systems, policies, and practices designed to prevent and respond to health threats. As you consider your part in this, you must acknowledge that robust health security contributes to societal resilience, enabling communities to withstand and recover from health shocks. The economic repercussions of health crises — whether through lost productivity, increased healthcare costs, or destabilisation of markets — highlight the pressing need for proactive measures to safeguard public health.
Current Landscape in Europe
On examining the current landscape of health security in Europe, it is evident that various challenges persist, particularly in light of recent global health emergencies. The COVID-19 pandemic illuminated significant gaps in preparedness and response mechanisms, revealing that Europe’s health systems often struggled to manage crises effectively. Moreover, the rise of antimicrobial resistance and climate change further complicates the health security framework, necessitating a comprehensive approach that encompasses not only immediate health responses but also long-term strategies to enhance resilience.
Consequently, European nations are re-evaluating their health security strategies, aiming to strengthen collaboration across borders and improve response frameworks. By investing in research, fostering communication among member states, and enhancing surveillance measures, you will find that the continent is gradually shifting towards a more integrated health security approach. It’s crucial to remain vigilant, as the volatility of health threats continues to escalate, making it imperative that you advocate for proactive policies that prioritise health security, thereby safeguarding your community and the wider society.
Political Frameworks for Health Security
If you are keen to understand how health security is effectively managed within European politics, you will find that it hinges upon robust political frameworks. These frameworks are largely shaped by the collaborative efforts of various institutions and national policies that seek to mitigate risk and enhance public health outcomes across the continent. As health crises can transcend borders, the response requires a coordinated political structure that not only addresses immediate threats but also prepares for future challenges by prioritising prevention, preparedness, and response strategies.
Role of European Union Institutions
At the heart of European health security lies the role of the European Union (EU) institutions, which are pivotal in formulating policies and programmes. The European Commission, for example, actively develops legislation aimed at harmonising health standards and ensuring that member states collaborate efficiently during public health emergencies. Additionally, the European Centre for Disease Prevention and Control (ECDC) plays a vital role in monitoring and reporting health threats, providing data-driven insights that help in shaping evidence-based decisions across the region.
National Policies and Collaborations
For you to fully appreciate the dynamics of health security in Europe, it is important to consider how individual nations contribute through their own policies and collaborate with each other. Each member state is responsible for implementing national health policies that align with EU regulations while addressing specific local health challenges. This dual approach allows for tailored responses that are both relevant and effective, fostering partnerships that enhance the overall response to health emergencies.
Considering the diverse healthcare systems and political environments across Europe, your awareness of how national policies are developed is imperative. These policies often embrace a multi-sectoral approach that involves not only health authorities but also various stakeholders, such as educational institutions and non-profit organisations. By leveraging local expertise and resources, nations can build agile collaborations that respond quickly to health threats and maintain a collective resilience against future risks. This synergy is paramount in fostering an interconnected health security landscape that can stand up to challenges that are intrinsic to the European Union as a whole.
Proactive Strategies for Risk Mitigation
Now, embracing proactive strategies for risk mitigation in health security is crucial in the evolving landscape of European politics. These strategies encompass a variety of approaches that aim to prevent, identify, and manage health risks effectively. By prioritising these methods, you can fortify your community against potential threats, ensuring a more resilient public health framework.
Surveillance and Early Detection
Surveillance systems play a vital role in monitoring public health trends and facilitating early detection of potential outbreaks or health crises. By investing in comprehensive surveillance programs, you enable health authorities to promptly identify emerging threats, ensuring that timely interventions can be implemented. This includes utilising technology and data analytics to track disease patterns and pinpoint unusual occurrences that could signify a developing health issue.
Public Health Infrastructure Enhancement
After establishing effective surveillance mechanisms, the next step is to enhance public health infrastructure. This involves strengthening healthcare systems, improving facilities, and expanding access to services. By investing in robust infrastructure, you ensure that health services not only respond swiftly to crises but also maintain a higher standard of care during normal operations. Your community will benefit from well-equipped hospitals, trained healthcare professionals, and efficient logistics systems that can adapt to various health challenges.
Considering the importance of public health infrastructure enhancement, you must focus on collaboration between government entities and healthcare providers. This collaboration can foster innovations in health delivery and expand training programs for healthcare workers, ensuring they are equipped to handle emergencies and everyday healthcare needs alike. By establishing a network of shared resources and seamless communication, you can significantly optimise health outcomes across Europe, paving the way for a healthier future for all citizens.
Cross-Border Cooperation
Once again, you are invited to consider the significance of cross-border cooperation in enhancing health security within European politics. This collaboration ensures that nations can jointly navigate the challenges posed by health crises, which frequently do not respect geographical boundaries. When countries work together, they can pool their resources, expertise, and knowledge to create more resilient health systems that can quickly respond to emerging threats. Your engagement in these cooperative efforts can lead to improved health policies and practices, benefiting not only your own nation but the entire European community.
Collaborative Health Initiatives
Collaborative health initiatives are vital for addressing health issues that affect multiple countries simultaneously. By participating in joint programmes, you can contribute to efforts aimed at combating infectious diseases, bolstering vaccination coverage, and developing strategies to handle public health emergencies. These initiatives often involve sharing best practices and lessons learned, allowing you and your neighbours to better equip yourselves against potential threats. The collective investment in these partnerships enhances the overall health security of the region and fosters a sense of solidarity among nations.
Information Sharing and Communication
Between nations, effective information sharing and communication are indispensable tools for enhancing health security. You must ensure that reliable and timely information flows seamlessly across borders, allowing for coordinated responses to health threats. Establishing robust channels for sharing data not only improves situational awareness but also enables you to respond more effectively to public health emergencies. This collaboration builds trust among countries, imperative for a unified approach to health security challenges.
Due to the interconnectedness of health concerns, the need for consistent communication among European nations cannot be understated. By sharing critical data on outbreaks, resource availability, and research findings, you will enhance your capacity to respond quickly and efficiently to potential threats. This reciprocal exchange strengthens the relationships between countries while fostering a climate of collaboration that can more effectively tackle future health emergencies, ultimately safeguarding the health of populations across Europe.
Addressing Socioeconomic Factors
All nations within Europe must take proactive measures to address the underlying socioeconomic factors that impact health security. By prioritising economic stability, equitable access to healthcare, and social welfare systems, governments can significantly improve the overall health of their populations. Here are some important steps that can be taken:
- Implement policies that promote economic equality.
- Enhance funding for healthcare services in underserved areas.
- Encourage community-based health initiatives.
- Support education programmes that raise awareness about health issues.
By focusing on these key areas, inequalities can be reduced, and the accessibility of healthcare improved, leading to more resilient communities. For more insight into this topic, visit Health Security means a Strong Europe. Knowing that your actions can help strengthen health systems across Europe brings an empowering sense of purpose.
Inequality and Accessibility Issues
About the disparities in healthcare access, it is important to recognise that health outcomes are often tied to socioeconomic status. Individuals from marginalised groups frequently experience barriers to accessing quality healthcare, which can lead to exacerbated health issues. Creating equitable healthcare frameworks requires understanding these inequalities and designing policies that address the unique challenges faced by disadvantaged communities.
Moreover, statistical data reveals that economic hardship significantly correlates with poorer health outcomes. By investing in comprehensive health services and equitable distribution of resources, your government can ensure that all citizens, regardless of their social standing, have the opportunity to achieve optimal health.
Community Engagement and Education
Beside addressing socioeconomic factors, fostering community engagement is vital for ensuring effective health security in Europe. By encouraging individuals to participate in local health initiatives, you can create a sense of ownership and responsibility towards personal and public health. Educational programmes can raise awareness about health topics and empower citizens to make informed decisions regarding their wellbeing.
Also, incorporating community feedback into health policies can lead to more effective strategies tailored to local needs. Promoting partnerships between government agencies, non-profit organisations, and community members fosters a comprehensive approach to health security, enabling everyone to play a role in enhancing public health outcomes.
Future Challenges and Opportunities
Keep in mind that the landscape of health security in Europe is continually evolving, presenting both challenges and opportunities that must be navigated wisely. As you engage with the ongoing discussions surrounding Health sovereignty, you will recognise that fostering resilient health systems is imperative. The interplay between national interests and collective action can either hinder or enhance the efforts towards a unified health strategy, which is vital for addressing emergent health crises effectively. By focusing on proactive steps that integrate diverse perspectives, you can contribute to a robust framework that anticipates future health threats.
Emerging Health Threats
One of the pressing concerns you must contend with is the rise of emerging health threats, including infectious diseases, antimicrobial resistance, and the impact of climate change on health systems. These threats often transcend national borders, necessitating a collaborative approach among European nations to share information swiftly and develop joint strategies. Strengthening surveillance systems, improving data sharing, and ensuring quick response mechanisms are imperative to mitigate the effects of these health challenges.
Innovations in Health Security
Behind the scenes, various innovations are revolutionising health security frameworks across Europe. From advanced technology in disease monitoring to novel vaccine development, you will find that these advancements can significantly enhance your nation’s health resilience. Embracing digital health solutions, including telemedicine and electronic health records, can streamline healthcare delivery and improve access, particularly during crises. These innovations not only foster greater efficiency but also empower individuals to take charge of their health.
Considering the potential of these innovations, it becomes evident that embracing a culture of collaboration and adaptability is key to navigating future health challenges. By prioritising investment in research, development, and technology, you can help create a health ecosystem that is not only reactive but also proactive. This ensures that European nations are equipped to respond effectively to unforeseen health threats while capitalising on opportunities that arise in an increasingly interconnected world.
To wrap up
With this in mind, you should appreciate the significance of proactive steps in ensuring health security within European politics. By advocating for policies that prioritise public health, you can contribute to a more robust framework that addresses both immediate and long-term health challenges. Engaging with health authorities and policy-makers not only amplifies your voice but also fosters collaboration across nations, enabling the sharing of best practices and resources. Your involvement in these discussions can drive the agenda towards sustainable health solutions that benefit all citizens.
Additionally, you may want to consider the importance of ongoing education and community engagement in fostering a culture of health security. By promoting awareness and understanding of health issues within your community, you can empower others to take part in preventive measures. Active participation in local health initiatives and supporting research can also strengthen the collective response to health threats. Ultimately, your commitment to these proactive steps can significantly enhance the health resilience of Europe as a whole.
FAQ
Q: What are the key proactive steps that can be taken to ensure health security in European politics?
A: Key proactive steps include enhancing surveillance systems to monitor health threats, improving intergovernmental cooperation among EU member states, investing in health infrastructure, and ensuring that healthcare policies are prioritised in political agendas. Furthermore, public health awareness campaigns can empower citizens to take action towards their own health security.
Q: How can European nations collaborate on health security?
A: European nations can collaborate on health security by establishing joint health initiatives, sharing data on health risks, and coordinating responses to health emergencies. This can be achieved through platforms such as the European Centre for Disease Prevention and Control (ECDC) and collaborative research projects that tackle shared health challenges.
Q: What role does funding play in health security within European politics?
A: Funding plays a significant role in health security, as adequate financial resources are necessary for effective health programmes, research initiatives, and emergency preparedness efforts. Governments should allocate appropriate budgetary resources to ensure that public health systems are resilient and capable of responding to crises.
Q: How can public engagement influence health security policies in Europe?
A: Public engagement is vital for shaping health security policies because it encourages transparency and responsiveness from policymakers. Facilitating open dialogues between citizens and government officials allows for valuable feedback and ensures that health policies reflect the needs and concerns of the population.
Q: What impacts does climate change have on health security in Europe?
A: Climate change poses significant risks to health security by exacerbating health issues such as respiratory diseases, heat-related illnesses, and the spread of infectious diseases. European politics must incorporate climate considerations into public health strategies to mitigate these risks and adapt health systems accordingly to endure the effects of climate change.
-
EU & the World4 days ago
Aurora Borealis Forecast: Where & When to See the Northern Lights Tonight
-

 Sports5 days ago
Sports5 days agoChampions League Final 2024-2025: PSG-Inter, official lineups
-

 EU & the World5 days ago
EU & the World5 days agoRihanna’s Parents: About Her Late Dad Ronald Fenty & Mom Monica Braithwaite
-

 Sports6 days ago
Sports6 days agoPSG-Inter, Nicolò Barella jokes about Gianluigi Donnarumma
-

 EU & the World7 days ago
EU & the World7 days agoHailey Bieber’s Net Worth: How Much Money the Rhode Founder Makes
-

 EU & the World7 days ago
EU & the World7 days agoHow to Get the Sydney Sweeney Soap: About the Dr. Squatch Product
-
 Politics6 days ago
Politics6 days agoEU and India Forge Deeper Maritime Ties with Historic Joint Naval Exercise in the Indian Ocean
-

 Sports6 days ago
Sports6 days agoPSG-Inter, Lautaro Martinez unveils recipe for finals